In the first in a series of articles I asked whether Omicron would drive a change in Hong Kong public health strategy. As anticipated the answer is yes. In a second article I considered what a Plan B may look like for Hong Kong. Although hard to believe, it appears that no coherent contingency plan was in place. We have now gradually transitioned towards mitigation. In the last article I asked whether dynamic zero Covid or mitigation was best for population health in Hong Kong. Unfortunately, the mortality data strongly indicates that the dynamic zero Covid approach was ultimately the wrong choice.
In this article, I ask how we got to this situation and how we should best proceed based on the assumption that the goal is to maximise the health and well-being of the population of Hong Kong.
Hong Kong currently has the highest per-capita mortality rates in the world, how did this happen?
Answer: We failed to vaccinate the most vulnerable members of our community.
As I have explained in previous articles the single most important intervention in Covid in population terms is vaccination and specifically vaccinations given from the most vulnerable down.
In the case of Covid the following are the public health priorities for Hong Kong, in order:
1. Increasing vaccine uptake in the old and vulnerable.
2. Increasing vaccine uptake in the old and vulnerable.
3. Increasing vaccine uptake in the old and vulnerable~October 21[1].
There is no evidence to suggest that the omicron BA.2 variant hitting Hong Kong is intrinsically any more serious than other Omicron variants. The impact on Hong Kong is due to three main factors:
-
- Low levels of natural population immunity
- Low levels of vaccine-induced immunity in the most vulnerable
- An overloaded health system
All of these factors were entirely predictable and are the result of previous policy decisions. This lack of foresight has shaped the challenging situation that Hong Kong is currently experiencing.
What a difference 2 months makes.

Fig 1. Cumulative confirmed COVID-19 deaths per million people from March 1, 2020 to January 9, 2022, featuring United States, United Kingdom, Europe, Singapore, Australia, Hong Kong, New Zealand and China.
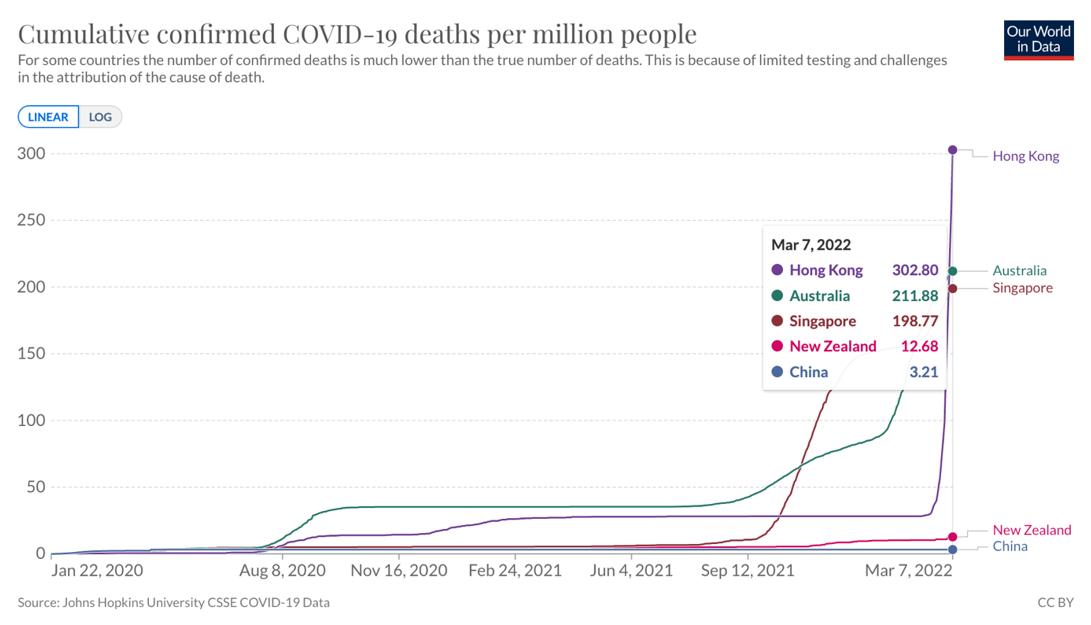
Fig 2. Cumulative confirmed COVID-19 deaths per million people from March 1, 2020 to March 7, 2022, featuring Singapore, Australia, Hong Kong, New Zealand and China.
Even using the most conservative predicted mortality data, Hong Kong is likely to end up with the highest per capita death rate in the elimination countries by some distance.
If the results were predictable, was this preventable?
Answer: Yes, this was preventable.
I explained in an article in June 2021 why zero Covid was not an effective long term strategy. Professor Ben Cowling and I also discussed the unsustainable nature of zero Covid, the inevitability of an exit wave and the importance of driving high vaccination rates in the vulnerable in a series of podcasts over the last year.
‘High vaccine coverage, especially for the vulnerable and a transition to living with Covid is ultimately the only viable long term solution.’
~ June 2021
One fundamental error over the last year was a focus on herd immunity as the primary goal of vaccination. Government medical experts (predominantly hospital rather than public health specialists) and media pushed the herd immunity narrative long after the science clearly showed that increasing transmissibility of variants made herd immunity impossible by vaccination alone.

Fig 3. '70% to herd immunity': A familiar refrain which is factually incorrect. 70% vaccination with a mixture of Sinovac and BioNTech vaccines alone will NOT be enough to reach herd immunity. This was misinformation.
Vaccinations are not as good at preventing Covid infections but they are fantastic at reducing the risk of people becoming seriously ill or dying.
'Explain to people we are not trying to get herd immunity, we are trying to stop Granny dying. The disease will come in, we can’t stop it'
One curious result of this strategy is that next week Hong Kong will almost certainly be the only country in the world having higher vaccination rates in ages 3-11 than in the over 80s.
If the science was so clear why did this happen?
Answer: Zero Covid without any exit plan is a bad strategy
Ultimately excess mortality in Hong Kong is caused by low vaccination rates in the vulnerable. We have good evidence from international studies that population vaccination rates are strongly correlated with trust in government and health institutions. In Hong Kong, the lack of any exit strategy resulted in a negative narrative focused on ‘keeping the bad guy out’. This created a climate of fear and encouraged rational vaccine hesitancy. The narrative around control and containment led to poor prioritisation and allocation of resources. Public health policy decisions increasingly became performative rather than substantive with very little, if any, grounding in science or evidence. The amount of energy and resources allocated to the upcoming compulsory universal PCR testing is an extreme example. I am not aware of one single expert in public health, family or community medicine, virology, medical administration or public policy who thinks that it is a good idea at this time. This includes the public health experts from China, for whom I have great respect and who have clearly indicated that resources and energy should be targeted towards minimising loss of life.
Performance over substance? Here are a few examples of some of the policies which were not grounded in science and likely did more harm than good.
- 21-day hotel quarantine
- Compulsory testing notices when testing and quarantine already overloaded
- Airline bans
- Border quarantine beyond time when it could make any difference
- Closing wet markets for deep cleaning
- Requiring masks whilst walking in the country park
- Taping off play areas and BBQ pits
So was elimination a bad idea?
Answer: No
In a previous article, I explained the difference between the public health strategies of elimination and suppress and lift. There is no question that the best strategy for managing Covid at the onset was elimination in order to protect the population until vaccinations were available. At that point the best strategy became very high vaccination rates across the population, especially from the most vulnerable down. For this strategy to be effective, it must be followed by communicating a plan for transition in order to prepare the population and the health system to move towards mitigation. The optimal time for this strategic shift in Hong Kong was the summer or autumn of 2021.
In summary, zero Covid with a planned exit was undoubtedly the best strategy for managing covid. Zero Covid without any exit plan is a bad strategy. In my opinion, it is likely that this strategy will end up being worse in terms of population mortality than countries that have been most effective in managing a suppress and lift strategy.
Why did Hong Kong ignore the science and continue with zero Covid with no exit plan?
Answer: Politics
China has a very strong tradition of public health. The policies undertaken in China have been extremely successful. At its most basic elimination requires three components.
-
- Test to identify cases
- Trace to identify contacts
- Isolation of contacts, to identify secondary infections and break transmission chains
This process breaks down when capacity at any point in the chain is exceeded. China has built enormous capacity in all areas. Factors within the political system, which includes high levels of trust in these policies, allows for rapid and high volume lockdowns. This is also facilitated by community organisations at district level in addition to widespread use of digital technology to identify potential contacts. It was always clear that Hong Kong lacked this capacity. As such we passed the critical threshold at which Omicron could be contained very early.
Whilst Hong Kong lacked capacity to eliminate we did have some potential advantages that favoured a transition to mitigation. We had early access to the most effective available vaccinations, a body of internationally renowned public health experts, a small geographic area with excellent hospital facilities and high-level medical expertise.
Notwithstanding the clear strategic and commercial value of the mainland border, the science suggested that by late 2021, if the only goal had been a focus on population health, then the best public-health strategy for Hong Kong was to maximise vaccination rates from the vulnerable down with the best available vaccines and use the same strategy as Singapore.
China has proven its ability to eliminate and the best strategy likely remains to continue elimination over the winter. The increasing transmissibility of the Omicron BA.2 variant means that continued elimination will be a challenge even for China. In my opinion, considering the availability of new anti-viral drugs and the proven effectiveness of vaccination I think it is most likely that China will begin to transition as early as Spring 2022.‘It may well be that elimination remains the best strategy for China because of factors in the political system in addition to the capacity and expertise in test, trace and isolate as a policy. In my opinion the cost of elimination exceeded the benefits to Hong Kong by mid to late 2021.’
In summary political imperatives failed to recognise the different structural capacities and threats in Hong Kong and China.
What is the best strategy for Hong Kong in the current context?
We can consider this question in two sections, short term and long term.
Short term
Answer: Minimise loss of life and protect the health system.
In the short term we must focus all of our energy and resources on minimising loss of life. This requires building out urgent care and ICU hospital capacity including using existing private facilities. Protecting the vulnerable as much as possible within their own environment or within other stepdown facilities or medical locations. Urgently procuring new anti-viral drugs and ensuring that the most vulnerable are vaccinated immediately. We should also stop wasting any time, energy and resources on policies which are not targeted towards these specific goals.
Long term
Answer: The only rational policy is a transition to living with Covid.
Positive communication and education are the key tools of epidemic control. We are not controlling Omicron, it is burning through in a wave. The wave was sharper and higher than in other locations, in part due to population density and overcrowding within our city but almost certainly also accelerated by policy decisions including crowds queueing for compulsory testing and sending positive patients to hospital and medical clinics. The result was a dramatic spike in infections, the vast majority of which were asymptomatic or mildly symptomatic. The wave will have mostly burned through by the end of March. We are likely already at herd immunity as our wave peaked a few days ago.
It is important to understand that herd immunity exists in a particular state. By mid-April we will have had something close to 5 million infections. This will be enough to bring the epidemic under control under the current social distancing regulations. If we were to immediately take off masks and move around the city as normal then the decline in infections may begin to plateau. We would continue to have some infections circulating and for this reason we still need to focus on boosting vaccination rates in the vulnerable and we will still need some mitigation for a few months in order to allow a gradual transition from around 70% immunity to closer to 90% population immunity. This would be the rational plan of a graduated transition to living with Covid. Under this scenario border controls are already unnecessary and they could certainly be removed by the end of March. There is no reason why our city could not be getting back to relatively normal life within 2 to 3 months.
An alternative scenario that has been discussed in the media is to use compulsory universal testing as a method of returning to zero Covid. It is important to realise that in a return to zero covid, especially in the context of immune waning, we could still experience a further surge in infections if we had imported cases again. In the context of an immune population, I can think of no scenario in which this would be in the best interests of population health in Hong Kong. In the short term it would do even more harm than it already has by diverting energy and resources from policies which are most effective in minimising loss of life. In the long-term it will damage population health through the inevitable social and economic damage of public health restrictions on our international city.
 Central General Practice
Central General Practice
 Repulse Bay
Repulse Bay
 Clearwater Bay
Clearwater Bay
 BodyWorX Clinic
BodyWorX Clinic
 Central Specialist Clinic
Central Specialist Clinic
 MindWorX Clinic
MindWorX Clinic
 Partner Clinics
Partner Clinics
 Family Clinic
Family Clinic
 OT&P Annerley Midwives Clinic
OT&P Annerley Midwives Clinic





