A timeline of the Hong Kong Public Health response.
The Covid-19 pandemic can be considered in two different phases: Pre-vaccine and post-vaccine. We have very good evidence that until the availability of vaccines, elimination was the best strategy. On this page I revisit a series of articles written since vaccinations became available in Hong Kong. I ask why Hong Kong failed to capitalize on the initial advantages of zero Covid and consider the factors which explain the significant increase in mortality in Hong Kong in the first quarter of 2022.
1. Pre-Vaccine
Early in the pandemic, there were broadly two strategies employed internationally.
-
- Elimination, that is zero Covid. The focus was on keeping the disease out of the territory. Test, trace and isolate with border quarantine.
- Suppress and lift. Public health measures were increased or reduced depending upon the rise and fall of infective waves in the population. In this context, public health restrictions were predominantly designed to take the pressure off health systems. This strategy was employed with varying degrees of success in different countries.
Pre-vaccines these were the only strategies available. We now have very good evidence that elimination was the best strategy. Mortality rates from countries which eliminated are significantly lower and in general, disruption to daily life and the negative impact on economic activity was also lower in the elimination countries.
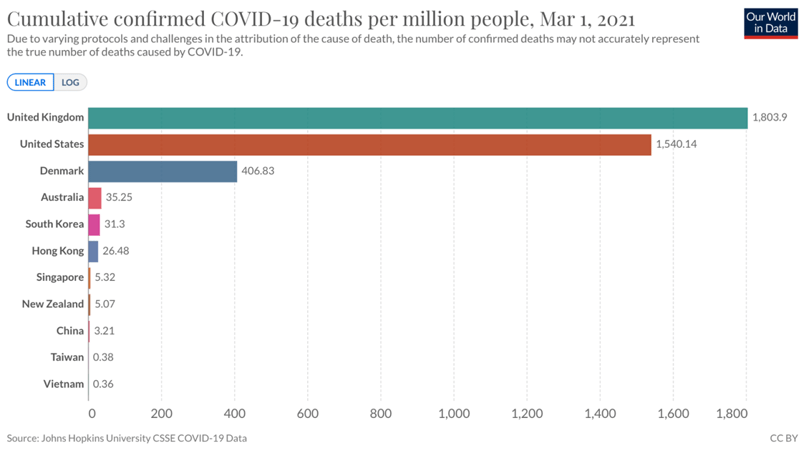
On March 1 2021, the HK vaccine program was rolled out online. The benefit was clearly visible in the total Covid deaths in the elimination countries. There was a significant discrepancy between countries which pursued suppress and lift strategies. Compare Denmark and the UK/USA at this time.
2. Post-Vaccine
Once effective vaccinations became available, a third option opened up. That is to vaccinate, to as high a proportion of the population as possible, preferably from the most vulnerable down and then to use public health measures to mitigate the final exit wave moving towards ‘managed endemicity’ or ‘living with Covid’.
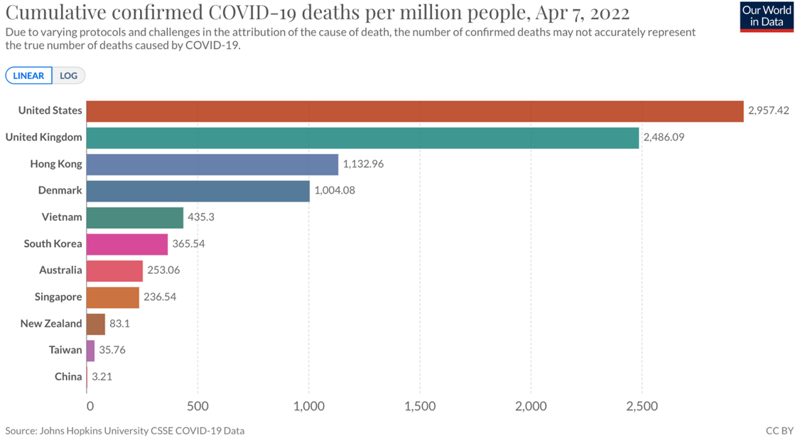
April 2022 much of the early benefit has been lost and Hong Kong has significantly higher cumulative mortality than other elimination countries.
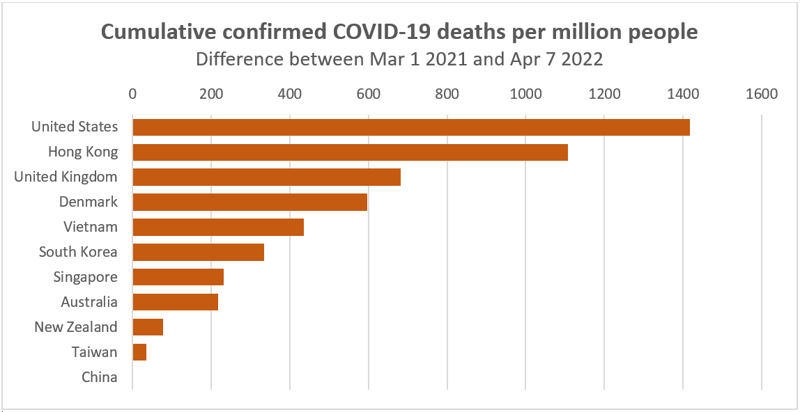
Population mortality since vaccines became available. The majority of deaths occurring in the last three months. Hong Kong has had the highest death rate in the world for the last 6 weeks.
Is Zero Covid a long-term sustainable strategy?
June 6 2021
In an article in June 2021 I explained the principles of elimination, I also explained why it was not a long-term sustainable strategy.
Although desirable, zero Covid is not a viable long term solution to the pandemic. The evidence would suggest that countries which excelled in implementing zero Covid as a short term policy, now need to focus on boosting vaccine uptake, and therefore immunity in populations.
Zero Covid has been a very successful strategy for Hong Kong but it was always a waypoint on the journey to population immunity via vaccination. Increasing vaccine uptake involves not only education but the explicit recognition that absolute risk can never be eliminated, it can only be mitigated.
High vaccine coverage, especially for the vulnerable and a transition to living with Covid is ultimately the only viable long term solution.
One consistent error in the Hong Kong public health response has been a failure to adapt to evolving evidence, indeed a tendency to pursue public health measures and restrictions at odds with the science used to justify them. By mid-2021 it was obvious that, whilst vaccinations are incredible at saving lives and reducing severe disease, they are less effective at preventing transmission. This meant that it would be impossible to achieve herd immunity by vaccination alone. The failure to accept, explain and adapt to the science is in large part responsible for Hong Kong having higher vaccination rates in ages 3-11 years than in ages 80+ despite the low vaccination in the elderly being the greatest threat both to the elderly but also to the young as we saw when the health system crashed.
Is it possible for Hong Kong to reach herd immunity?
June 25 2021
It is almost certainly not possible to get to herd immunity with vaccination alone. However, vaccines are extremely effective in protecting individuals. The higher the level of vaccine immunity, the less pressure there will be on hospitals and healthcare workers
Herd immunity by vaccination alone is impossible. We need to vaccinate the vulnerable
July 30 2021
Note that in the intervening month ‘it is almost certainly not possible’, had become, ‘it is not possible’. This was based on evolving evidence of increasing infectivity of the virus in addition to the evidence of lower antibody levels and faster waning of immunity with Sinovac. Even at this point there was a push to vaccinate both children and young adults whilst ignoring the overwhelming threat of low vaccination rates in the vulnerable.
It is not possible for Hong Kong to achieve herd immunity by vaccination alone. Locations that seem to be close to herd immunity have acquired this population immunity from a combination of immunisation and infections.
High vaccine coverage is a good thing. If Hong Kong vaccinated 100% of the population, people would be safe because 100% of the population would be protected individually by vaccination. Unfortunately we will not be able to vaccinate 100% of the population. Apart from vaccine hesitancy, we cannot yet vaccinate young children.
Hong Kong needs to challenge the current narrative that focuses on the purpose of vaccinations as primarily being to lead to herd immunity. We need to move away from the false assertion that vulnerable members of our community will be safe when the population vaccination level hits 70% and towards an emphasis on the importance of this population getting vaccinated so that they are protected when the disease inevitably gets into our city.
Is Hong Kong’s 21-day Quarantine evidence-based or justified?
October 7 2021
The use of quarantine and border controls, along with the separation of children from their parents, have been the most contentious issues in the Hong Kong response. Many of these decisions have been unscientific and ethically questionable. They also increased the risks to population health.
Ultimately all epidemics of infectious diseases require a balance between the cost of the disease (human and economic) and the social, economic and political costs of the public health interventions. Restriction of movement and quarantine are decisions which balance the rights of the individual against the rights of the majority.
Excessive public health controls have the potential to do harm directly and indirectly. In the case of quarantine, directly in that the statistical probability of hotel acquired infections in 21-day quarantine, is greater than it would be for 14-day quarantine and almost certainly exceeds any potential benefit of the extra week. That is to say 21-day quarantine actually increases the risks to the population. Even more important is the negative impact on the overall public health strategy.
In the case of Covid the following are the public health priorities for Hong Kong, in order:
1. Increasing vaccine uptake in the old and vulnerable
2. Increasing vaccine uptake in the old and vulnerable
3. Increasing vaccine uptake in the old and vulnerable
There is no scientific evidence to support 21-day quarantine. It is neither evidence-based nor proportionate and is almost certainly doing more harm than good.
Covid vaccine mandates the arguments for and against
December 7 2021
By early December 2021 the threat from Omicron was clear.
The single greatest threat to Hong Kong is the low vaccination rates in the most vulnerable members of our population. Currently only 18% of the over 80s are vaccinated. This population are 600 times more likely to die and 15 times more likely to require intensive care treatment than a young person. It is important to appreciate that this threat is not only to the elderly themselves. Covid has the potential to overwhelm the health system leading to significant mortality in the wider population. The increase in mortality in Covid waves results from a combination of increasing mortality attributable to both Covid and other medical conditions.
Vaccine mandates specifically targeting the elderly and most vulnerable are an ethically justifiable intervention in order to increase vaccination rates and to protect other members of the population vaccinated and non-vaccinated, both young and old.
Omicron in Hong Kong: Will The Public Health Policy Change?
January 13 2022
It is hard to argue against the success of elimination early in the pandemic. However, elimination was always a holding strategy, buying time to achieve high population immunity via vaccination. We have increasing evidence from South Africa, the UK, EU and recently from the USA,[1] that despite rapid surges of Covid the incidence of death and serious disease due to Omicron is significantly lower than from previous variants. All these countries have high levels of immunity from a combination of previous infections and vaccination. There is a suggestion that the impact of Omicron is greater in locations with lower levels of existing immunity. In this regard lessons from Singapore and Australia are very important. These countries, like Hong Kong, were essentially infection naive. So far the data provides reason to be cautiously optimistic that transition from zero Covid is possible without losing the historical population benefit. An exit wave and further deaths are likely whether or not the transition is planned or accidental. This point must be recognised and communicated. Not least because Hong Kong has an already overloaded health system, lower vaccination rates (especially in the most vulnerable) and more widespread use of less effective vaccines than Singapore or Australia. We will need to mitigate an evolving Omicron wave to a greater degree.
Hong Kong Covid Strategy: Will It Adapt To Change & Is There a Plan B?
January 25 2022
Structural issues in the political systems and populations mean that both the socioeconomic impact and the capacity to eliminate Covid are different in Hong Kong and China. Omicron may yet escape even the ability of China to eliminate. Regardless of the political and economic benefits of an open border, the science has for some time suggested that population health in Hong Kong would be best served by a different strategy. Why has this science not driven policy to a greater degree?
In the last three months vaccination rates in the most vulnerable have increased from 15% to 30%, yet this remains amongst the lowest in the developed world. Apart from negatively impacting vaccination rates, our focus on locking down borders to keep the disease out has been associated with negative messaging and blame. The current outbreak was entirely predictable, it was triggered by a non-evidence-based 21-day hotel quarantine policy. A narrative built around creating scapegoats, whether it be aircrew or hamsters, shifts the emphasis away from an evidence-based focus on policies supported by science.
What could Plan B look like?
Answer: Mitigating the impact of Omicron on the health system and accepting a transition to ‘Living with Covid’.
1. Positive communication and education
2. Drive vaccination rates
3. Social distancing restrictions
4. Removal of close contact quarantine and hospitalisation of all cases
5. Pivot to home rapid testing
What next for Hong Kong: Dynamic zero or mitigation?
February 17 2022
Answer: Mitigation is not only the most rational option for Hong Kong. It is the only option.
In the early stages of the pandemic elimination was the best strategy. At some point, the cost of elimination in terms of both public health measures, but also the risk to population health, exceeds the costs of a mitigation strategy. It may well be that elimination remains the best strategy for China because of factors in the political system in addition to the capacity and expertise in test, trace and isolate as a policy. In my opinion the cost of elimination exceeded the benefits to Hong Kong by mid to late 2021.
The most important priority in any public health strategy is to define the public health goals, develop strategies to best achieve those goals then positively communicate the actions needed to achieve them. Failing to explicitly define and explain a policy has the potential to be actively harmful to population health.
As an example, in an elimination strategy, it may make sense to keep asymptomatic people in hospital to minimise the risk of community spread. In mitigation, we need to prepare our hospitals to treat sick people. It may seem counterintuitive, but in a Covid pandemic the last place we want infectious people is in hospitals, unless they really need treatment. The vast majority of people can be managed at home.
The large numbers of people in queues for compulsory testing and especially the people being sent to hospital with positive rapid tests both significantly increased the risk of an accelerating epidemic. We are already seeing a sharp rise in illness and isolation in healthcare workers. It seems inconceivable that the health system can continue for long without a change in strategy.One urgent priority is to transfer asymptomatic and mildly symptomatic patients out of the hospitals and preferably to home, or to government facilities when home is not possible. The recent images of patients waiting outside hospitals are disturbing and create anxiety. The hospitals are currently overcrowded partly because we have admitted people who don’t really need to be there. Over the next few weeks they will become full of people who really do need to be there.
Failure to vaccinate high levels of the elderly and vulnerable was ultimately responsible for a significant amount of the excess mortality in Hong Kong. However, the failure to have a backup plan and in particular the delay in pivot towards mitigation, ultimately overloaded the hospital system and resulted in a significant number of unnecessary deaths.
How did we get here and what next for the Hong Kong Covid strategy?
March 9 2022
Hong Kong currently has the highest per-capita mortality rates in the world, how did this happen?
Answer: We failed to vaccinate the most vulnerable members of our community.
There is no evidence to suggest that the omicron BA.2 variant hitting Hong Kong is intrinsically any more serious than other Omicron variants. The impact on Hong Kong is due to three main factors:
1. Low levels of natural population immunity
2. Low levels of vaccine-induced immunity in the most vulnerable
3. An overloaded health system
All of these factors were entirely predictable and are the result of previous policy decisions. This lack of foresight has shaped the challenging situation that Hong Kong is currently experiencing.
Ultimately excess mortality in Hong Kong is caused by low vaccination rates in the vulnerable. We have good evidence from international studies that population vaccination rates are strongly correlated with trust in government and health institutions. In Hong Kong, the lack of any exit strategy resulted in a negative narrative focused on ‘keeping the bad guy out’. This created a climate of fear and encouraged rational vaccine hesitancy. The narrative around control and containment led to poor prioritisation and allocation of resources. Public health policy decisions increasingly became performative rather than substantive with very little, if any, grounding in science or evidence.
Why did Hong Kong ignore the science and continue with zero Covid with no exit plan?
Answer: Politics
In summary political imperatives failed to recognise the different structural capacities and threats in Hong Kong and China.
The strategy that must not be named
March 25 2022
If our actions point to living with Covid does it matter what we call it?
Answer: Yes it very much matters how we define our strategy
The Hong Kong Covid response has been defined by a mixed narrative rather than a clear strategy. The continued focus on herd immunity by vaccination is one good example. Basing our policies on a percentage of the total population being vaccinated makes no scientific sense. It is one of our policy errors. Vaccinations are not as good at preventing Covid infections but they are fantastic at reducing the risk of people becoming seriously ill or dying.
The focus on the biologically impossible concept of herd immunity by vaccination alone led us to drive vaccination rates in the young rather than to address the elephant in the room, which was the unvaccinated vulnerable.
We must protect the vulnerable, both young and old. It is a balance. The Hong Kong Covid strategy has been based upon the illusion of the total elimination of all risk. Risk can never be eliminated, it can only ever be mitigated. Every public health intervention carries a cost and unintended consequences. I am not advocating for open borders to make holiday travel and life easier for expatriates. Excessive focus on the risks of the disease ignores the potential impact on the rest of the population. Pandemics always aggravate the impact of social inequality. The poorest children fall behind in education and the lowest-paid workers are most likely to be both unemployed and impacted (physically and psychologically) by the disease. In population terms, poverty and social inequality are the greatest drivers of poor health. The damage caused to population health in Hong Kong at this stage of the epidemic will be significantly greater from the economic impact of the public health measures than from the disease itself.
It is now clear that many decisions in Hong Kong were made for political rather than public health reasons. The result of these policy decisions can be clearly measured by looking at the differential mortality rates between Hong Kong and Singapore. One of the most important lessons to take forward from the last year is that ignoring evidence-based public policy decisions in favour of politics is very bad for public health.
For anyone interested in exploring these issues in more detail within the context of the evolving epidemic, we produced a series of Podcasts which are all available on the link above, or via your preferred podcast provider.
 Central General Practice
Central General Practice
 Repulse Bay
Repulse Bay
 Clearwater Bay
Clearwater Bay
 BodyWorX Clinic
BodyWorX Clinic
 Central Specialist Clinic
Central Specialist Clinic
 MindWorX Clinic
MindWorX Clinic
 Partner Clinics
Partner Clinics
 Family Clinic
Family Clinic
 OT&P Annerley Midwives Clinic
OT&P Annerley Midwives Clinic





