Updated on March 26th 2020, written by Dr David Owens.
Containment versus management, understanding the process of the epidemic and the reasons for the public health measures.
I have explained in a previous article the importance of understanding infectious illnesses in terms of information relating to the disease and information relating to the epidemic. In population terms the impact of infectious diseases will be driven by the epidemic process. A severe disease which is relatively contained (SARS mortality rate 9.8% killed 800 worldwide) will have significantly less impact than a less severe disease which spreads widely (Influenza mortality rate 0.1%, kills up to 650,000 every year from respiratory disease alone1.
Ultimately all epidemics of infectious diseases require a balance between the cost of the disease (human and economic) and the economic and political costs of the public health interventions. The principle of public health interventions in epidemic control has been explained previously. The control of new infectious diseases involves relearning the lessons of the past. By definition, when new infectious diseases arise we don’t have information about their severity, about their methods of spread and we don’t have treatments immediately available. This means that the first strategy is one of containment. Methods of containment invariably involve political decisions. Restriction of movement and quarantine are decisions which balance the rights of the individual against the rights of the majority. This process can be critiqued in philosophical and political terms. There have been criticisms that public health interventions have been both slow and inadequate but also that they have been excessive. As an example of opposing perspectives here is an analysis from a traditional Western perspective2 yet the public health interventions in China have been described by the Director General of WHO as an “unprecedented response” he further praised the “extraordinary measures it (China) has taken to contain the outbreak despite the severe social and economic impact”. I am a doctor with a community health bias. It is neither within my remit nor am I trying to make any political points. However, it is important to appreciate that control of infectious disease, by definition, has a significant political and economic component and the narratives around the management of infectious disease must be understood in this context.
When does containment end?
In a previous article, I explained the process of the epidemic using the analogy of a fire. I will continue this theme to illustrate the transition from the containment phase to that of ongoing management which involves a shift towards control and mitigation.
Think of this epidemic as being like a fire which started to rage in Wuhan. We didn’t have methods to put out the fire (drugs to treat the illness) so we needed to focus on containment. The fire will need to burn out by itself. Sometimes nature helps us, although in the case of a coronavirus it is sunshine and heat that help to put out the fire rather than rain. This is how the public health measures work. We build a wall around the fire to contain it. As often happens in this situation some embers escape. Some land on the ground and burn out but others start smaller, little fires. Fortunately, because the alarm has sounded everybody is now aware and focused on the new outbreaks and it is usually easier to contain small fires than big ones. There is a danger that an ember lands in a particularly dry and vulnerable place and triggers another larger fire (or series of small fires). We can consider that this has happened on the cruise ship, in Iran, Korea and Italy. How well the fires are contained in new locations will depend on a number of factors, including population immunity, environmental and political factors which influence the ability of the medical firemen to do their job of containment and the capacity of the health system to manage the resulting complications of the illness. Infectious diseases (fire in this analogy) always do the greatest damage in poor communities with low capacity health systems.
To expand this analogy, when this fire (the disease) first broke out we had no idea how bad it would be on a case by case basis. I have explained previously the dilemma of predicting the severity of a disease early in epidemics. The first doctors in China who saw this disease were worried that SARS had returned and the first series reported from Wuhan had an 11% mortality. Although there is much to learn, we now know much more than we knew then. This is certainly an important disease but it doesn’t cause severe disease in children, it seems to have a lower mortality than first feared and although it is obviously quite infectious in certain circumstances evidence of infections exported from China suggested that 89% of embers did not cause another fire. Although we are seeing infections from individuals who have no, or minimal symptoms, it seems that the majority of infections are spread by individuals with symptoms and this would generally be positive in terms of the potential impact of public health measures. Again, I wish to emphasize that if this disease really is as infectious as some of the rapidly evolving clusters suggest it may be in certain circumstances, then it must have a lower fatality rate on a case by case basis.
When the fire first broke out the containment response meant stopping people around the fires moving so that they didn’t spread the fire (restriction of movement and quarantine). The principle then would be to do the same thing around all the smaller fires. The containment response also involved reducing risk by closing schools and reducing population mixing (restricting crowds and working from home) which as I have explained is like spraying water on the ground to reduce the risk of embers catching.
Early in the process it seemed reasonable to advise people to not move and stay in their fire proof homes. Obviously, the firemen (doctors, nurses, workers in energy and transport) need to keep working throughout. But what happens if the fire seems to be coming under control or what if the fire seems to be dangerous but only in certain circumstances? It is well recognised that poverty is the single biggest factor that determines health in population terms. At some point, we need to keep the economy functioning or more people will die as a result of the economic fallout than from the impact of the disease. This is the dilemma of negotiating the transition from the early aggressive containment phase to managed containment and eventually, depending on the unfolding scenario of the epidemic, either back to the old normal, or the new normal of control and mitigation. I have explained a previous article the importance of data in assessing the progress of the epidemic (the size of the fire). Many newspaper and media reports focus on cumulative data. Below are typical examples:
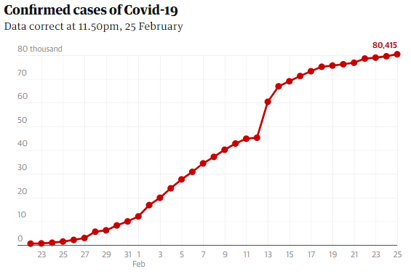
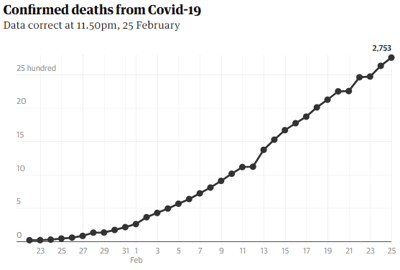
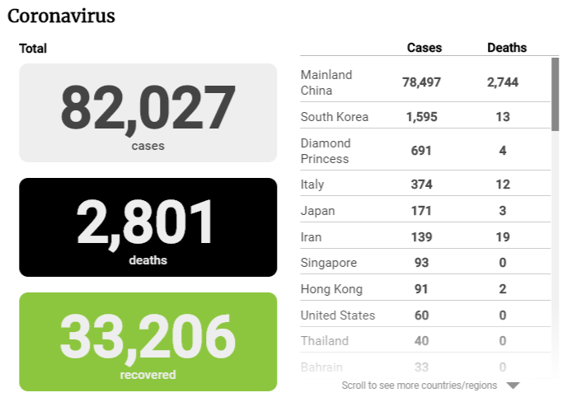
This process of focusing on the mortality of the disease without comparison or context reinforces anxiety and confounds understanding. Unless people begin undying the deaths will only rise and the number of cases can only fall if they have been misdiagnosed.
How do we place 20,339 worldwide deaths from a new disease in context? How about in comparison with other established infectious diseases? In a typical year the annual global mortality from some common diseases is below3:
Measles: 140,000 deaths
Influenza: 650,000 deaths
Tuberculosis: 1.5 million deaths
Infectious gastroenteritis: 1.8 million deaths
Much more relevant in the understanding of a new disease is the change in incidence over time. This leads to the concept of the epidemic curves. They tell us how the epidemic is evolving and give information as to whether the fire is getting bigger or smaller. These curves apply to different clusters and reflect the fact that fires are burning with different size and intensity in different locations.
Below is the epidemic curve for Guangdong4:
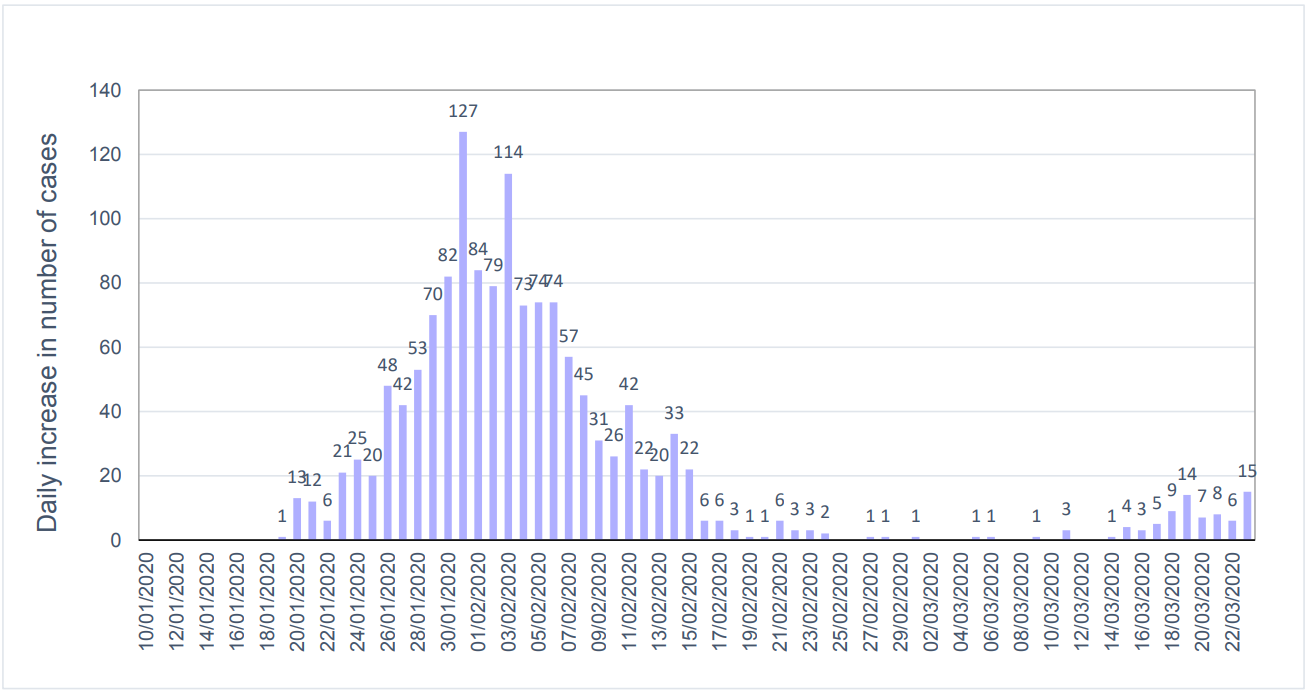
Figure 1: Daily number of newly confirmed cases reported in Guangdong Province since January 10, 2020
This is why China is currently in the process of returning to work. This suggests that in Guangdong at least the fire is coming under control. Containment strategies are still in place although they vary depending on location and based upon a balance between the risks of the fire and the health risks to the population of an impact on economic activity.
This is how the WHO describes the evolution of epidemics of infectious disease5.
Containment: Effective and rapid containment of emerging diseases is just as vital as early detection in order to avoid a large scale epidemic. Rapid containment should start as soon as the first case is detected regardless of the etiology, which is most likely to be unknown. It requires skilled professionals to safely implement the necessary countermeasures. Pre-training of these professionals is essential to guarantee the safety and efficiency of the operations.
Control and mitigation: Once the infectious disease threat reaches an epidemic or pandemic level, the goal of the response is to mitigate its impact and reduce its incidence, morbidity and mortality as well as disruptions to economic, political, and social systems.
Elimination or eradication: Control of a disease may lead to its elimination, which means that it is sufficiently controlled to prevent an epidemic from occurring in a defined geographical area. Elimination means that the disease is no longer considered as a major public health issue. However, intervention measures (surveillance and control) should continue to prevent its re-emergence.
So what happens next?
There is a spectrum of potential scenarios for the evolution of this epidemic. For simplicity I will describe the range as below:
- Best Case: The disease is ultimately shown to have a low mortality (<1%) the numbers of cases and deaths remains small in comparison to other diseases such as influenza and it dies around Spring (like SARS) or later, and never comes back.
- Intermediate Case: By definition a wider range with increasing numbers and fatalities either due to worse disease severity or increased epidemic size and geographic spread (epidemic versus pandemic) and/or a disease which stays and becomes endemic or goes and returns in the future. This scenario would be the one which would ultimately respond best to a vaccine.
- Worst Case: The disease mutates and produces a more severe illness and/or a greater capacity to spread. Whilst the most severe outcome the natural history of Coronavirus and other viral illness is that viral mutation typically reduces rather than increase in severity over time.
Whilst accepting the inevitable uncertainties involved in this evolving process the current data is suggestive of an outcome which is more likely to be closer to the best case than the worst case scenario. The impact in population terms (exactly where on the spectrum we end up) will depend on the evolving epidemic and in particular on the containment strategies in newer locations (Iran, Korea, Italy, Japan). If the disease spreads widely it may well be declared a pandemic. This essentially means that there are fires in multiple locations. H1N1 (Swine flu) was declared a pandemic in 2009. It is important to appreciate that controversy around the declaration of a pandemic is similar to the initial decision to label COVID-19 as a global emergency. There will be political factors in the decision which again balance the benefits of the release of funding and human capital against the increasing anxiety, confusion and potentially harmful decisions which may result in a label which has negative connotations beyond its meaning on the ground.
So how do we get back to work?
Managing this process will be a matter of assessing the epidemic data and managing the evolving risk/benefits in the context of competing needs of the population. This will require a change in messaging and an explanation of the reasons for public health decisions.
The WHO makes this statement about communication in epidemics:
This is why risk communication, a set of sophisticated skills, is increasingly employed by health authorities, agencies, physicians and professional health personnel. It is more important now than ever to learn and apply them. The latest and most accurate information must be conveyed frequently, and uncertainties related to an epidemic must be acknowledged in order to maintain credibility and public trust.
Strong and coordinated public messaging is easier in systems with either central control or significant political capital. This epidemic has been subject to over reach at an international, national, business and individual level. Examples include the unilateral closure of borders, restriction of travel, suspension of airline routes and restrictions on work and social activity beyond those advised by experts in public health.
One of the best examples of this dilemma is the question of masks. The same issue played out during SARS. It is pretty much universally accepted in public health circles that the single most effective intervention in droplet borne infections is hand washing. Masks are not recommended in low risk situations by the WHO and most other international public health bodies6. Standard advice would be to wear a mask if you are ill, caring for someone who is ill or for high risk contact such as health care workers. This was the public health decision made in Singapore. The counter argument is that masks may still give some benefit, even if only stopping facial touching, they are more socially acceptable in Hong Kong and really at the end of the day even if they don’t make a significant difference what harm can they do?
Every public health intervention has a risk and a benefit. There are three further arguments against masks:
- Moral Hazard: The single most effective intervention to prevent COVID-19 is handwashing. Don’t confuse the key public health message.
- Resource Issues: We have long queues of people, standing in groups waiting to spend too much money on an overpriced resource with minimal benefit, increasing their risk of infection meanwhile there is a worldwide shortage of masks for health care workers such that the WHO has been forced to make recommendations on the dangers associated with misuse7.
- Signalling: Accepting the social norm in Hong Kong a mask is a very clear signal that something bad is happening. The lack of smiles and social interaction is very unhealthy in population terms.
The decisions on masks can be considered a surrogate for other public health decisions. Doing ‘a little bit more’ than is recommended to be ‘a little bit safer’ can create unexpected, unpredictable and often significant impact on social and economic life. It is like building the wall too far out from the fire. The result is that some people are impacted unnecessarily and everybody gets a bit more scared that the fire is coming for them. It also means that people are unable to work and eventually society cannot afford to pay the firemen.
Getting back to work will involve a shift in messaging. It will require an explanation of the changing public health strategy. Using my metaphor this will involve taking the wall from around Hong Kong and accepting that whilst little fires may continue to break out we are fortunate to have one of the best medical fire departments in the world. We will likely move to local containment, continuing with quarantine around infectious clusters. Eventually offices will need to get back to work and children will need to go back to school. The decision to delay school opening until after Easter makes perfect sense in population terms. Two weeks off school buys four weeks in which we can spray water on the ground to reduce risks of seeding and enhance existing containment strategies. This does not reflect a worsening of the disease or an increase in local risk. It is likely that working practices will begin to revert to normal over the next few weeks. We will all eventually, both literally and metaphorically need to take our masks off, start smiling at each other and focus on health not disease.
I want to emphasize that COVID-19 is a new and emerging global health threat. New diseases always do the greatest harm in poor communities and low capacity health systems.
The international containment efforts so far have been unprecedented. They have at the very least delayed the spread of the disease giving greater time for understanding. Research is underway looking at both treatments and the development of a vaccine. I fully support the public health goals and continue to believe that Hong Kong has world class systems and expertise in the control of infectious disease. This disease, whilst severe in certain circumstances, seems generally less severe than was first thought. It will have greatest impact on older people with coexisting illness. As previously discussed, COVID-19 is not a form of influenza. We have a vaccination and treatments against influenza. However, in decisions involving risk the human brain is wired to mix up the severity of an event and the risk of the event. We need an anchor to put our risk in context. This disease has so far affected 435,625 people and killed 20,339. This compares to influenza which in the United States alone has infected 38 - 54 million people and killed 23 - 59 thousand since 1st October 2019. There have so far been 411 cases in Hong Kong out of a population of 7.4 million. The impact of COVID-19 on our population will be determined by the epidemic, not by how severe the disease is on a case by case basis. Returning to normal will be determined by an increasing understanding of the epidemic and a balance between the threat of the disease and the cost of the public health controls in both human and economic terms. The move to local containment and mitigation and control will involve a shift in messaging and will require education and communication.
Click here to learn more about the latest on COVID-19.
All our public health information regarding COVID-19 is also available in Chinese here.
References
1. Paget, J., Spreeuwenberg, P., Charu, V., Taylor, R. J., Iuliano, A. D., Bresee, J., … Global Seasonal Influenza-associated Mortality Collaborator Network and GLaMOR Collaborating Teams*. (2019, December). Global mortality associated with seasonal influenza epidemics: New burden estimates and predictors from the GLaMOR Project. Retrieved February 26, 2020, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6815659/#R2
2. Institute of Medicine (US) Forum on Microbial Threats. (1970, January 1). Strategies for Disease Containment. Retrieved February 26, 2020, from https://www.ncbi.nlm.nih.gov/books/NBK54163/
3. World Health Organization. (2018, May 16). Mortality and global health estimates. Retrieved February 26, 2020, from https://www.who.int/gho/mortality_burden_disease/en/
4. (2020). Retrieved 5 February 2020, from https://www.chp.gov.hk/files/pdf/statistics_of_the_cases_novel_coronavirus_infection_en.pdf
5. World Health Organization. (2018). Managing epidemics: Key facts about major deadly diseases. Retrieved February 26, 2020, from https://www.who.int/emergencies/diseases/managing-epidemics-interactive.pdf
6. World Health Organization. (n.d.). When and how to use masks. Retrieved from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/when-and-how-to-use-masks
7. World Health Organization. (2020, February 27). Rational use of personal protective equipment for coronavirus disease 2019 (COVID-19). Retrieved March 2, 2020, from https://apps.who.int/iris/bitstream/handle/10665/331215/WHO-2019-nCov-IPCPPE_use-2020.1-eng.pdf
 Central General Practice
Central General Practice
 Repulse Bay
Repulse Bay
 Clearwater Bay
Clearwater Bay
 BodyWorX Clinic
BodyWorX Clinic
 Central Specialist Clinic
Central Specialist Clinic
 MindWorX Clinic
MindWorX Clinic
 Partner Clinics
Partner Clinics
 Family Clinic
Family Clinic
 OT&P Annerley Midwives Clinic
OT&P Annerley Midwives Clinic
 WellWorX Clinic
WellWorX Clinic






