Between January and March 2022, I published a series of articles asking, 'What next for the Hong Kong Covid response?' In this article, I consider whether the new administration is living up to the promise of a more science-based approach. Whilst it is early days, the most recent policy changes do not support this assertion.
Hong Kong recently reduced border quarantine. The explanation given for the current '3 + 4' policy was that after 3 days, the prevalence of imported positive cases was equal to the background prevalence in the community.
Question: Can the current border quarantine policies be justified on the basis of science?
Answer: No. There is no scientific basis for any continued quarantine in Hong Kong at this stage of the pandemic. We have a highly immune population.
The argument used to justify the '3 + 4 policy' is reductionist. It ignores the following important issues.
1. What is the cost of quarantine to both the economy and public health?
Answer: Continued border quarantine will have a significant negative impact on the economy. At this stage of the epidemic, these policies will do significantly more long-term harm to population health than the disease itself.
2. What difference will quarantine make to population Covid mortality, if any?
Answer: Almost no difference at this stage of the pandemic.
3 If the population risk of an individual after 3 days of quarantine is the same as any random member of the HK population, is there any justification for the traffic system?
Answer: No.
Covid reality: Hong Kong and China are at different stages of the pandemic.
In a previous article, I asked why the clear advice of Hong Kong’s public health, epidemiology and virology experts has not driven a science-based strategy.
In summary political imperatives failed to recognise the different structural capacities and threats in Hong Kong and China.
We have very good evidence that Zero Covid was the best public health response before the availability of vaccines. China has consistently demonstrated an extraordinary ability to maintain elimination despite increasingly transmissible variants. This ability was influenced by capacity in testing, tracing and isolation in addition to structural factors within the political system. Ultimately, permanent elimination of Covid is impossible and, at some point, a transition to endemicity will inevitably occur in China.
Hong Kong is in a very different situation compared to China. Regardless of the political imperatives, Hong Kong was unable to maintain Zero Covid and as a direct result, has high levels of hybrid immunity due to a combination of high levels of vaccination and natural infection. There is no rational scientific argument in this context for a continued elimination strategy and to continue with such policies is actively harmful to population health in Hong Kong.
On October 7th, I wrote an article on the 21-day quarantine policy implemented in Hong Kong at that time. I posed the following question:
Question: Surely it pays to be prudent. Is longer quarantine not safer?
Answer: No
'All public health interventions, as with all medical interventions, involve a risk-benefit analysis. Doing a little bit more to be a little bit safer has the potential to produce unintended consequences and the possibility to increase harm. Continuing antibiotics for a little bit longer or in a slightly higher dose to ensure the infection has been eradicated increases the risks of drug resistance which increases the long-term risk to the population. Doing extra tests or scans leads to unnecessary biopsies and procedures, this has the potential to do more harm than good to the individual and increase costs to the health system. Excessive public health controls have the potential to do harm directly and indirectly. In the case of quarantine, directly in that the statistical probability of hotel acquired infections in 21-day quarantine, is greater than it would be for 14-day quarantine and almost certainly exceeds any potential benefit of the extra week. That is to say 21-day quarantine actually increases the risks to the population. Even more important is the negative impact on the overall public health strategy.
In the case of Covid the following are the public health priorities for Hong Kong, in order:
1. Increasing vaccine uptake in the old and vulnerable.
2. Increasing vaccine uptake in the old and vulnerable.
3. Increasing vaccine uptake in the old and vulnerable.
Unfortunately, Hong Kong failed to modify public health policies in response to evolving evidence.
How did Hong Kong perform in comparison to other countries?
Covid can be considered to be a pandemic of two stages, pre- and post-vaccine. The evidence is clear, elimination policies resulted in the lowest mortality in the initial pre-vaccine phase. By the time vaccinations were introduced into Hong Kong in February 2021, Hong Kong had amongst the lowest mortality rates in the world.
Today, Hong Kong has overall Covid mortality rates which are by some distance the worst of the initial elimination countries and in the middle of the pack when looking at countries which eschewed early elimination. Our response was not as bad as the UK or US but much worse than Singapore and Japan.
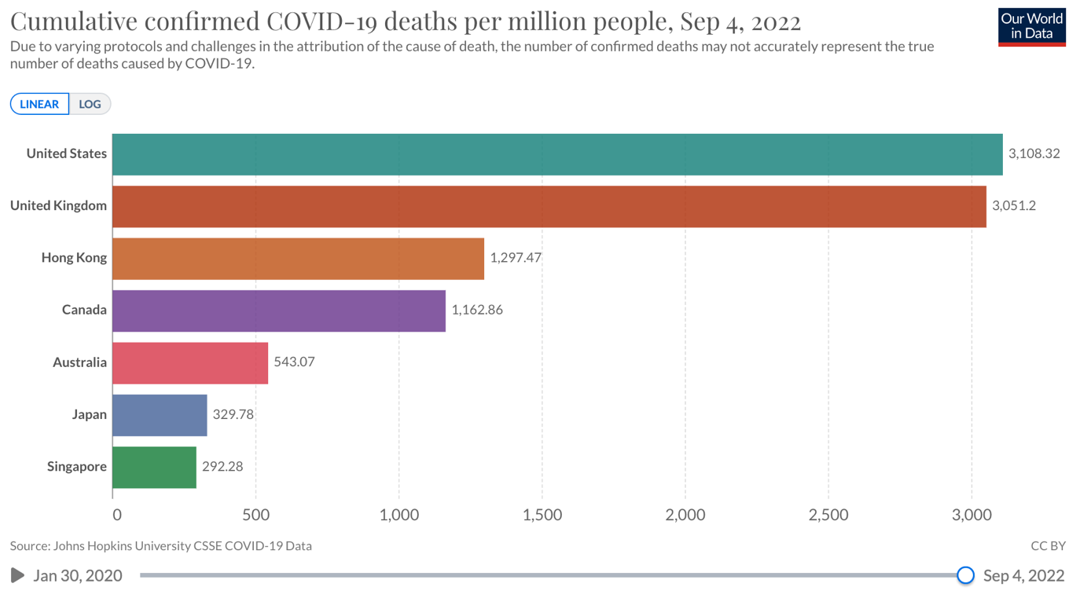
Fig 1. Comparison of cumulative mortality between open and early elimination countries
Here is how we compare with our Asia-Pacific neighbours.

Fig 2. Comparison of cumulative mortality between Hong Kong and neighbouring countries
Hong Kong is relatively wealthy, has excellent infrastructure, a strong reputation for virology and public health and had early access to vaccines. We made the right decision to close the border and pursue elimination. However, Hong Kong performed poorly in the post-vaccine phase of the pandemic. In the last 12 months, Hong Kong has had Covid mortality rates amongst the highest in the developed world. Worse than both the US and the UK.
Below is the cumulative mortality per million people over the last 12 months.
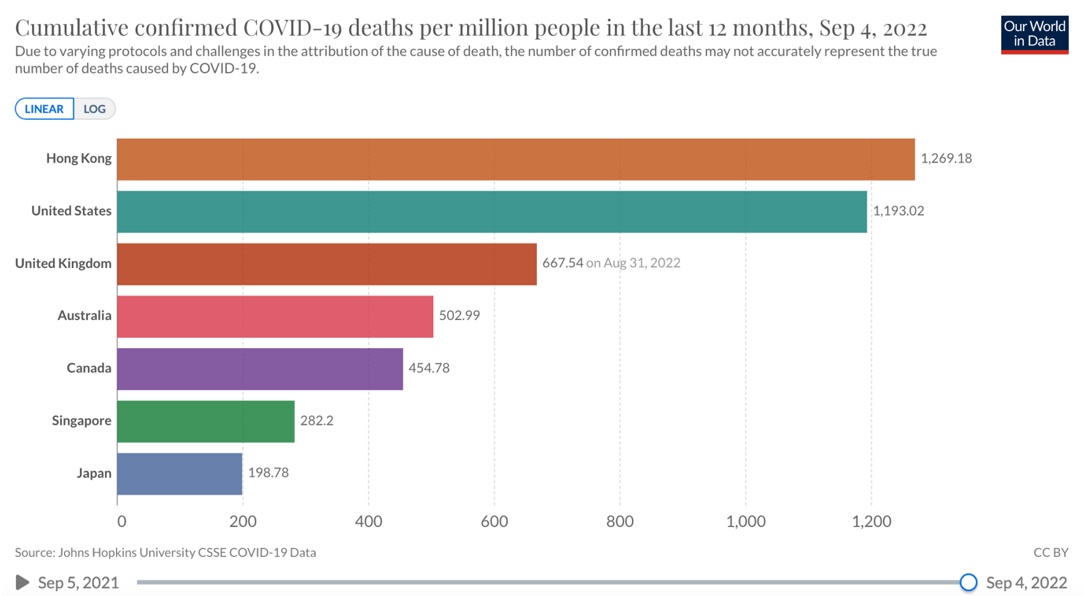
Fig 3. Cumulative mortality from Covid over the last 12 months
Of course, there is more to population health and population mortality than Covid. Below is a graph of population mortality in Hong Kong between 2016 - 2022. Analysis shows >11,600 excess deaths in Hong Kong between March - August 2022. The original data is available here[1]. This compares to a total of 9,724 cumulative deaths reported from Covid.

Fig 4. Excess mortality in Hong kong 2016-2022. Graph and data courtesy of Joel Chan @kjoules
How can excess mortality be explained?
Similar findings have been described in other parts of the world. Understanding the factors behind excess mortality is complex. Mortality rates are influenced by socioeconomic and demographic factors within and between populations. These factors include poverty, social inequality, age, obesity, incidence of other medical conditions etc. In addition to system based differences in reporting.
It is also important to consider factors within both health systems and public health responses. In this regard considering the performance of similar populations making different policy choices can be helpful. Below is a comparison of cumulative mortality between Hong Kong, Singapore and Japan.
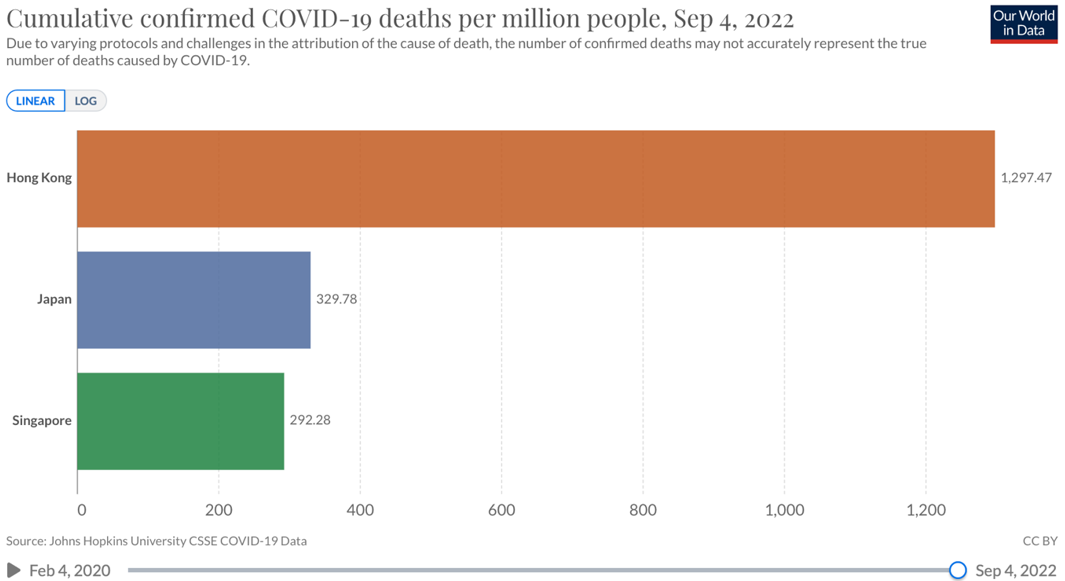
Fig 5. Comparison of cumulative mortality between Hong Kong, Singapore and Japan
Direct comparison between Hong Kong and Singapore may be confounded to some degree by different standards of reporting Covid deaths. Crude analysis suggests that pro rata Hong Kong had an excess of around 7 - 9,000 deaths. The recent suggestion that the excess mortality in Hong Kong was due to the higher proportion of elderly in the Hong Kong population is not supported by evidence.
How can the difference in mortality between Hong Kong and Singapore be explained?
Excess Covid mortality in Hong Kong was caused by two factors:
- We did not vaccinate the most vulnerable.
- Our health system was overloaded increasing all-cause mortality.
One way of considering excess deaths when comparing locations with different policy responses is:
- Inevitable Covid deaths even with optimal public health policies.
- Inevitable deaths indirectly related to Covid even with optimal public health policies.
- Excess Covid deaths due to sub-optimal public health policies.
- Excess non-Covid deaths due to sub-optimal public health policies.
It is a hard reality that some deaths from Covid are inevitable. This will, unfortunately, include some young people. Whilst we should do everything possible to minimise Covid mortality, pretending it is possible to totally eliminate all risk is bad science and dangerous misinformation. Covid is a multi-system, inflammatory, pro-thrombotic condition. Clearly, we should try to minimise the disease burden in population terms, but in any widespread epidemic, we will see increased mortality from secondary causes such as heart attacks, strokes etc. Some extra deaths will be inevitable regardless of what public policies we put in place.
Sub-optimal policies undoubtedly increased both Covid and non-Covid deaths in 2022. The factors leading to low vaccination in the vulnerable are complex and multifaceted but include poor communication, the pursuit of the illusion of zero risk, a culture of fear and control rather than education, an excessive emphasis on quarantine rather than vaccination and an irrational focus on population based herd immunity rather than a focus on vaccinating the vulnerable. Whilst the failure to vaccinate the most vulnerable put significant pressure on the hospital system, policy decisions around December 2021 - February 2022, especially the focus on the prospect of compulsory universal testing and the continuation of compulsory testing notices in addition to the hospitalisation of all positive cases led to a failure to pivot long after the system had broken down. These decisions led to crashing of the hospital system and a significant increase in mortality.
Finally, one side effect of Zero and Dynamic Zero Covid policies has been to effectively close down other hospital services. Hospitals were previously occupied by healthy people who stayed for weeks. Currently, a major reason for stress in the hospital system is that mostly elderly people with mild symptoms or placement issues are nursed in specialist units. This drains resources from other key health services. It will be some time before the true toll in excess mortality from undiagnosed cancer, heart disease etc is known.
In summary, both Hong Kong and Singapore used elimination policies pre-vaccination. Subsequently, Singapore made science-based public policy decisions grounded in and reacting to evolving evidence.
So what does the science tell us?
We now have a much greater understanding of the biology and epidemiology of Covid. As previously described Covid can be considered in two distinct stages:
- Pre-vaccine
- Post-vaccine
Mortality from Covid has dropped by greater than tenfold as a result of vaccination, natural immunity and improved treatments. This is obviously good news. However, from a population health perspective, we now know that herd immunity will not eliminate the disease. What we are seeing is the continual evolution of variants being driven by immune escape. The new variants develop an ability to dodge existing immunity. We will continue to see waves of infections, likely occurring 4 - 6 monthly, at least initially. The frequency of recurrent infections (the attack rate) means that although on a case-by-case basis the disease for most people will be mild, Covid will continue to be a burden on population health. Fortunately, at least so far, immunity against death and severe disease is very well preserved. For this reason public health policies should focus on the incidence of severe disease and the stress on the health system rather than attempting to identify and control every infection. The majority of current Hong Kong policies continue to focus on controlling infections. Indeed the current stress on the healthcare system in Hong Kong is mostly a direct result of hospital policies which focus on infection control rather than disease management. A focus on infections rather than disease makes no sense in the context of the existing high levels of population immunity. The current sixth wave will burn through Hong Kong over the next 4-6 weeks despite, not because of, current policies. The policies will have minimal influence on the total number of infections which will be brought under control by population immunity. Hybrid immunity, access to anti-viral medications and the evidence-based deployment of vaccinations represent the evidence-based management of Covid in 2022. A good summary of the role of hybrid immunity, written by experts from HKU (including members of the government expert medical committee) was published in July 2022[2].
'Thus, the most reasonable course of action is to achieve hybrid immunity as soon as possible so that life can go back to normal.'
'To achieve the most protective hybrid immunity before winter so as to avoid another catastrophic collapse of our healthcare system, we should continue to relax gradually our social-distancing measures so that the background immunity of our population against severe Covid is constantly boosted by natural infection with Omicron sub-variants including BA.2, BA.2.12.1, BA.2.75 or BA.4/5, while we await an Omicron-specific booster.'
Not lying flat
Public health is about much more than Covid. Accepting the reality of the science of Covid and instituting evidence based Covid strategies which ensure that other public health functions remain fully supported is not 'lying flat'. Ultimately all public health interventions are a balance between the costs of disease in human and economic terms and the costs of the public health measures. This is not an argument for lives or the economy. This is an argument for lives or lives. All public health interventions have consequences both positive and negative. A number of government officials have recently stated that any death of a child is a tragedy. I agree, these are amongst the most difficult situations that I have faced in my career in medicine. However, it is innappropriate to use scare tactics to justify public health policies which can not be supported by science. Many policies implemented in Hong kong have targeted and impacted children who have an inherently very low risk of severe complications of Covid. This is especially the case for otherwise healthy children with existing immunity. To focus specifically on the small number of deaths in children from Covid is to ignore the bigger picture. The goal of public health should be to make decisions that do the greatest good for population health. These policies should be communicated positively. As an example a review of child deaths in Hong Kong between 2016-2018 found 259 youth and child deaths of which 59 were due to suicide[3]. Numerous recommendations were made in order to target prevention strategies around non-natural deaths. The majority of these interventions were relatively low cost around education. How many lives could be saved if we invested a fraction of the current resources spent on PCR testing into evidence-based accident and suicide prevention strategies? A UNICEF study estimated that more than 240 thousand child and maternal deaths in South Asia in 2020 occurred as a direct result of disruption to healthcare services caused by Covid restrictions[4]. This is significantly more than caused by the disease itself. I would be very surprised if the same impact on maternal and child health is not the case in Hong Kong. This is before we even consider the costs in terms of damage to educational and social development. Pandemics increase social inequality and have the greatest impact on the poor and vulnerable. Poverty and social inequality are by far the greatest drivers of population health. If Hong Kong really does not want to 'lie flat' we should start making public policy decisions which are grounded in science. This would allow us to utilise the enormous resources which are currently employed in Covid theatre and focus on evidence-based interventions which impact social inequality in addition to tackling the underfunding and structural inequities which place our health system under chronic stress.
Reference
1. Hong Kong Monthly Digest of Statistics 香港統計月刊. (n.d.). Retrieved September 6, 2022, from https://www.censtatd.gov.hk/en/data/stat_report/product/B1010002/att/B10100022022MM07B0100.pdf
2. Beyond Hong Kong's Covid-19 Fifth Wave: Coping with the Coronavirus. AsiaGlobal Online Journal. (n.d.). Retrieved September 6, 2022, from https://www.asiaglobalonline.hku.hk/beyond-hong-kongs-covid-19-fifth-wave-coping-coronavirus
3. Fifth Report of Child Fatality Review Panel released (with photo). The Government of Hong Kong Administrative Region - Press Releases. (n.d.). Retrieved September 6, 2022, from https://www.info.gov.hk/gia/general/202111/23/P2021112300246.htm
4. UNICEF. Direct and indirect effects of the COVID-19 pandemic and response in South Asia. (n.d.). Retrieved September 5, 2022, from https://www.unicef.org/rosa/media/13066/file/Main%20Report.pdf
 Central General Practice
Central General Practice
 Repulse Bay
Repulse Bay
 Clearwater Bay
Clearwater Bay
 BodyWorX Clinic
BodyWorX Clinic
 Central Specialist Clinic
Central Specialist Clinic
 MindWorX Clinic
MindWorX Clinic
 Partner Clinics
Partner Clinics
 Family Clinic
Family Clinic
 OT&P Annerley Midwives Clinic
OT&P Annerley Midwives Clinic
 WellWorX Clinic
WellWorX Clinic





