Education and information are crucial factors in the management of infectious disease. The distinction between the disease and the epidemic is key.
Updated 7 April 2021
In infectious disease the uncertainties can broadly be divided into two completely different but related issues.
1. The Disease Process: This helps to address the question:
-
- What will happen to me if I get sick?
2. The Epidemic Process: This deals with the questions:
-
- How likely am I to get sick now?
- Will that change in the future?
More on COVID-19
We prepared a comprehensive list of our resources related to the novel Coronavirus:
- Podcast Update: 25 February 2021
- COVID-19 Vaccinations in 10 Easy Questions
- Update on Vaccines for COVID-19
- Testing for COVID-19
- COVID-19 Vaccination: A Survey of OT&P Patient Perceptions
- COVID-19 Timeline: OT&P Communication
What do we know about the disease?
We continue to get more data and information from locations with different strategies in managing the pandemic. Medical research is being shared and published internationally. I will continue to update this information in terms of:
The Disease: What will happen to me or my family if we catch this virus?
The Epidemic: How likely am I to catch this virus and is that risk changing?
The Disease
We now have a much greater understanding of this disease. There is a consensus of three potential stages. The first stage, the incubation period, patients typically have no symptoms, they may or may not have detectable virus. Individuals may be infectious from 2-3 days before they develop symptoms. Many people recover without progressing. The second phase involves symptoms, typically not severe, the virus will be detectable. Most people will never get past this stage and will recover. In the third stage, there is the development of increasingly severe inflammatory or infective symptoms, especially involving the lungs. This leads to increasing cough and shortness of breath. This stage is associated with increasing viral load. In some patients this stage is associated with an excessive immune reaction which may lead to a ‘cytokine storm’. This is an overwhelming internal battle which can lead to damage not only to the lungs but other organs. Part of this immune response is targeted against blood vessels. The immune reaction of blood vessels leads to an increase in blood clotting which plays a role in the damage to organs within the body. One rare but important example of this tendency has been the increase in Kawasaki disease in children[1].
In addition to older males with other illness the disease is more serious in health care workers (because of viral load) and in association with obesity and poverty. Studies in the UK and US also show a significantly higher incidence in people from Black, Asian and Ethnic Minority (BAME) backgrounds. It is unclear yet the relative contribution of genetic, economic and social factors but it is already clear that COVID-19 will amplify social inequality. Poverty is associated with both higher infection rates and worse outcomes. One simple way of thinking about this process is that COVID-19 is generally worse as biological age increases. It is important to appreciate that individuals do not age biologically at the same rate. We can control some factors which influence the biological ageing process. Obesity, poor diet, lack of exercise and metabolic syndrome make people old before their time and these conditions significantly worsen outlook in COVID-19. An early review in the Lancet looked at outcomes in critically ill patients. The mean age in this cohort was 60 with 67% males. The authors concluded that ‘the severity of SARS-CoV-2 pneumonia poses great strain on critical care resources in hospitals, especially if they are not adequately staffed or resourced[2]. This message was reinforced in a further paper in the Lancet looking at the Italian experience[3]. The mean age of death in Italy was 81 years. This varied from 83.4 years in females to 79.9 years in males. There was a 4 to 1 ratio of males to females. Two thirds of fatalities had other medical conditions or were smokers. Between 9-11% of patients admitted to hospital required intensive care treatment.
There are now numerous trials of drug treatments. The WHO maintain a consensus position on internationally reputable trials. A recent review in the British Medical Journal summarised the latest evidence[4]. The only drug which has been proven to be effective in COVID-19 is Dexamethasone (a steroid) and this is really only recommended for significant or severe disease. This emphasizes the importance of adequate research before drugs are widely recommended for treatment of new diseases. More high quality peer reviewed studies on intervention, such as those performed in Hong Kong, are needed internationally.
Test, trace, isolate and the use of intermittent enhanced social distancing measures has been shown to be highly effective in controlling the impact of COVID-19 on the Hong Kong Health system. It has however resulted in a significant economic cost. The management of any infectious epidemic as a balance of the lives lost due to the disease itself (and especially in COVID-19 due to the overwhelming of health systems) versus the harm done and the lives lost due to the economic impact of the public health measures. Immunisation offers the best chance to escape the current suppression but there is again a balance to be achieved in terms of the choice of new vaccines and the speed and prioritisation of the population immunisation program. The Hong Kong Government has announced the procurement of three different vaccine candidates which will be dependent upon peer reviewed evidence from ongoing studies. This makes perfect sense. Voluntary immunization programs rely upon trust in Health institutions in addition to logistical factors including manufacture, procurement, delivery, cold storage and ultimately vaccination. We have produced a separate article on COVID-19 vaccines which we will continue to update as evidence accumulates.
As we have previously explained questions about the disease relates to the question what happens if something bad happens to me or my family? These are What If? questions. In order to understand the risk of this bad thing happening we need to replace these questions with What is the risk of catching COVID-19? To answer this question we need information. When we are dealing with uncertainties it helps to have an anchor for risk. In order to assess this risk we need to understand the epidemic.
The Epidemic Process
To understand the risk of catching COVID-19 we need to understand the epidemic.
In a previous article we explained the principles of the public health measures.
In any infectious virus the following factors influence the size of the epidemic:
- Mode of Spread
- Incubation Period
- Infectivity in the Incubation
- Individual and Population Immunity
These factors ultimately lead to a basic reproduction number R0 for each illness. This number is a measure of on average how many people are infected by an individual with the specific disease. If this number is <1 the epidemic will die (this means that on average each infected person infects slightly less than one other person). If this number is >1 the epidemic is likely to grow. Infections with higher R0 values are more likely to spread. Population measures such as isolation of infected individuals, masks, hand washing, school closures and social distancing all work by reducing the exposure risk with the intention of reducing the effective R0 below 1 but regardless as much as possible in order to give the best possible chance for the epidemic to die. We now have good evidence that public health controls based on the principles of social distancing can reduce R0 and control epidemic spread. The balance between the costs and benefits of public health controls will be key in controlling the epidemic. Hong Kong University measures the effective R0 in Hong Kong. It is available here[5]. This is a good measure of the impact of the current public health measures in Hong Kong in real time.
Understanding epidemics is maths and data. Try to look at the change in cases rather than cumulative cases. The number of cases and the number of deaths will get bigger every day. It is the rate of change which tells us whether the epidemic is getting bigger or smaller. Epidemic curves are useful to get a sense of where the fires are burning and most importantly whether that intensity is increasing or reducing as this will determine risk. It is important to realise that even within countries, we are not dealing with one big fire, but lots of little clusters which may be very distinct in the risk that they pose. Remember too that death is a lagging indicator. People must first get sick, they are then usually diagnosed and either recover or in some cases die.
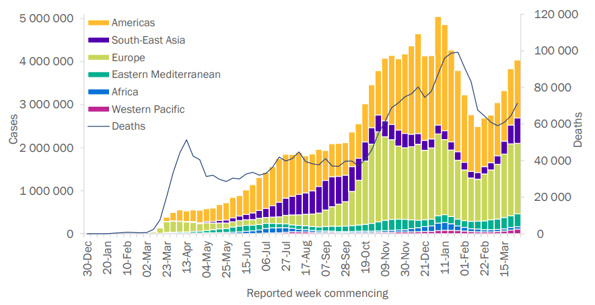
Figure 1 - Epidemic curve of confirmed COVID-19, by weekly date of report and WHO region through 4 April 2021[6].
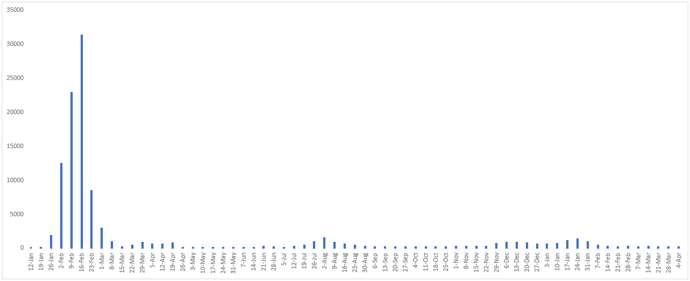
Figure 2 - Weekly number of newly confirmed cases reported in Mainland China since January 12, 2020. Including the case revision on 4 April, 2021.
Figure 3 is the latest data from the epidemic curve for Guangdong.
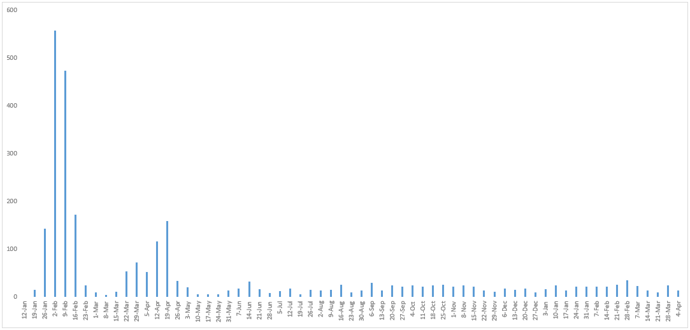
Figure 3 - Weekly number of confirmed cases reported in Guangdong Province since Janaury 12, 2020.
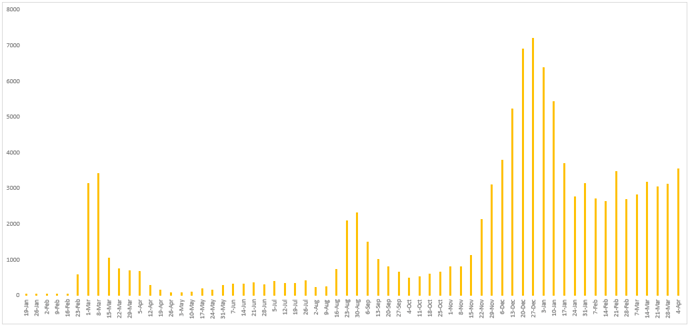
Figure 4 - Weekly number of newly confirmed cases reported in South Korea since January 12, 2020.
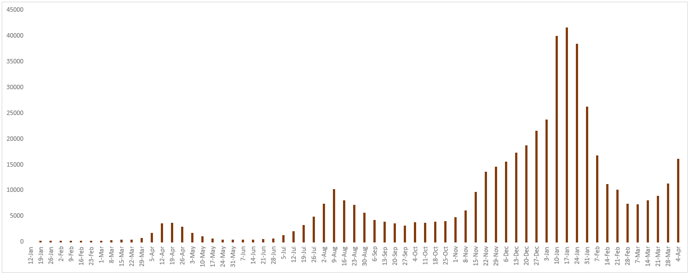
Figure 5 - Weekly number of newly confirmed cases reported in Japan since January 12, 2020.
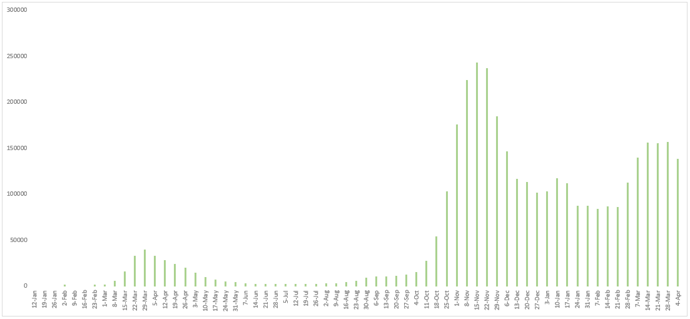
Figure 6 - Weekly number of newly confirmed cases reported in Italy since January 12, 2020.
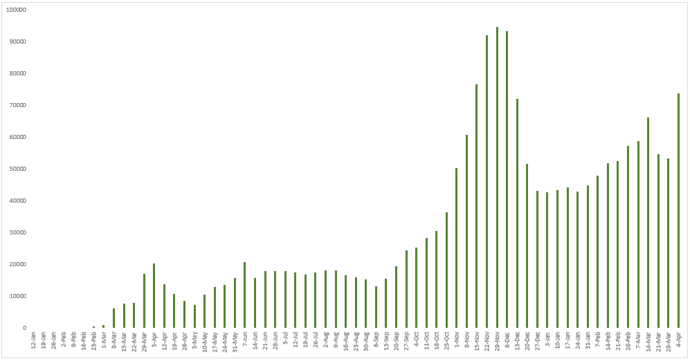
Figure 7 - Weekly number of newly confirmed cases reported in Iran since January 12, 2020.
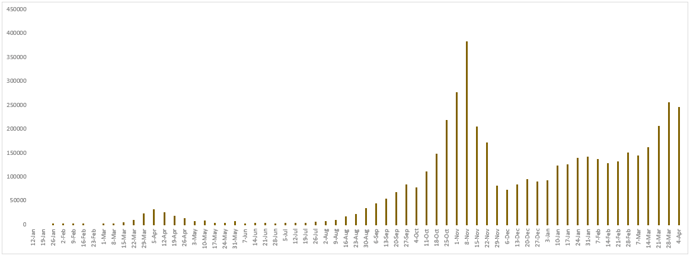
Figure 8 - Weekly number of newly confirmed cases reported in France since January 12, 2020.
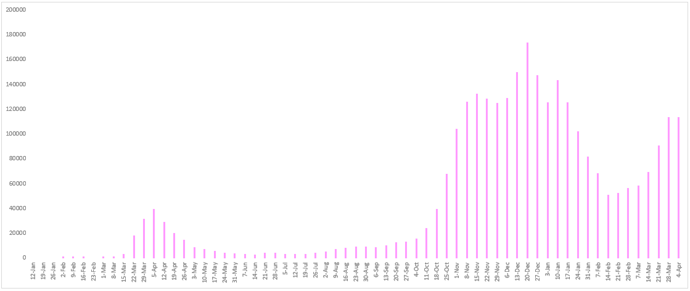
Figure 9 - Weekly number of newly confirmed cases reported in Germany since January 12, 2020.
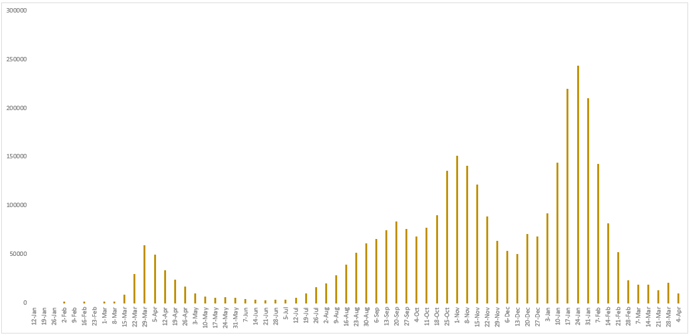
Figure 10 - Weekly number of newly confirmed cases reported in Spain since January 12, 2020. As of April 26, 2020, Spain has revised its cases to only PCR-positive cases, reducing their numbers by 12,130.
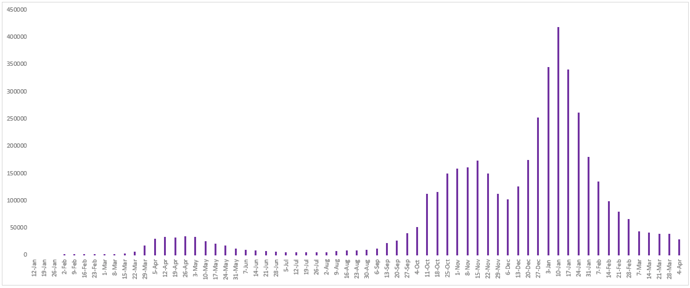
Figure 11 - Weekly number of newly confirmed cases reported in the United Kingdom since January 12, 2020.
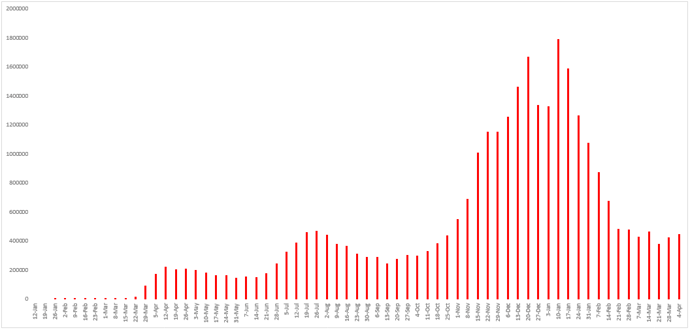
Figure 12 - Weekly number of newly confirmed cases reported in the United States since January 12, 2020.
Ultimately the impact of this disease on the population will be driven by the evolution of the epidemic. Excessive focus on the disease has the potential to distort real risk and significantly increase anxiety for the reasons previously discussed.
We will continue to update the article as data becomes available and information changes.
To learn more about the explanations behind the current public health measures, please click here.
References
1. Verdoni, L., Mazza, A., Gervasoni, A., Martelli, L., Ruggeri, M., Ciuffreda, M., . . . D'Antiga, L. (2020, May 13). An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: An observational cohort study. Retrieved September 07, 2020, from https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31103-X/fulltext
2. Yang, X., Yu, Y., Xu, J., Shu, H., Xia, J., Liu, H., . . . Shang, Y. (2020, February 24). Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Retrieved September 07, 2020, from https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30079-5/fulltext
3. Remuzzi, A., & Remuzzi, G. (2020, March 13). COVID-19 and Italy: What next? Retrieved September 07, 2020, from https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30627-9/fulltext
4. Siemieniuk et al. (2020, September 04). A living WHO guideline on drugs for COVID-19. Retrieved December 21, 2020 from https://www.bmj.com/content/370/bmj.m3379
5. Real-time dashboard. (n.d.). Retrieved September 07, 2020, from https://covid19.sph.hku.hk/
6. WHO. (n.d.). Coronavirus Disease (COVID-19) Situation Reports. Retrieved April 7, 2021, from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
 Central General Practice
Central General Practice
 Repulse Bay
Repulse Bay
 Clearwater Bay
Clearwater Bay
 BodyWorX Clinic
BodyWorX Clinic
 Central Specialist Clinic
Central Specialist Clinic
 MindWorX Clinic
MindWorX Clinic
 Partner Clinics
Partner Clinics
 Family Clinic
Family Clinic
 OT&P Annerley Midwives Clinic
OT&P Annerley Midwives Clinic
 WellWorX Clinic
WellWorX Clinic






